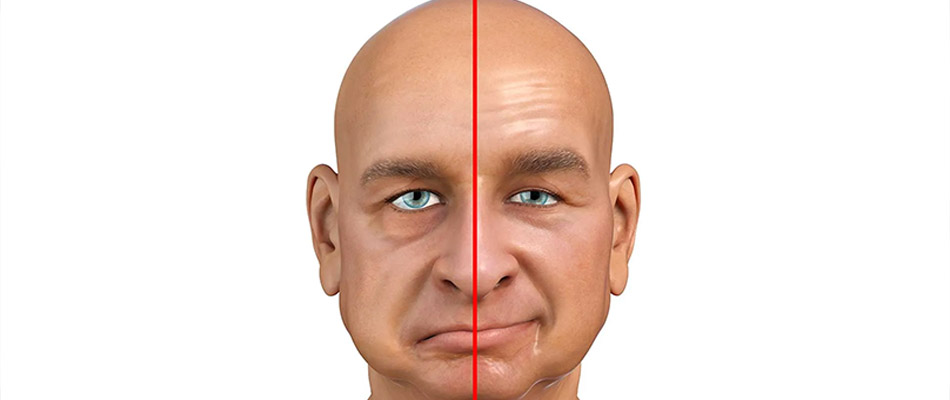
Bell’s Palsy is a condition characterized by the sudden onset of facial paralysis or weakness, typically affecting one side of the face. Although the exact cause is not entirely understood, it is often associated with viral infections and inflammation of the facial nerve. In this article, we will explore the nature of Bell’s Palsy, its possible causes, how it is diagnosed, the range of treatment options available, and what the future may hold for those affected by the condition.
What Is Wax Therapy?
Bell’s Palsy is a form of temporary facial paralysis resulting from inflammation or compression of the seventh cranial nerve, known as the facial nerve. This nerve is responsible for controlling the muscles of facial expression, and when it becomes inflamed, it can lead to a sudden, sometimes severe, weakness or paralysis on one side of the face.
The condition was first described by Sir Charles Bell, a Scottish surgeon, in the 19th century. While its sudden onset is alarming, most patients recover fully, often with minimal residual effects. However, the experience can be distressing due to the physical appearance changes and the functional limitations it may impose, such as difficulties with eye closure, eating, and speaking.
Anatomy and Function
The facial nerve is a mixed nerve that not only controls the muscles involved in facial expression but also carries fibers that are responsible for taste sensations on the anterior two-thirds of the tongue, and it plays a role in the production of saliva and tears. Because of its multiple functions, inflammation or compression of the facial nerve can have several clinical manifestations beyond mere muscle weakness.
Pathophysiology
The exact mechanism underlying Bell’s Palsy remains a subject of ongoing research. The prevailing theory is that the condition is caused by an inflammatory reaction—often following a viral infection—that leads to swelling within the narrow bony canal through which the nerve passes. This swelling compresses the nerve fibers, interfering with the transmission of nerve signals to the facial muscles. When the nerve is compressed, the result is the sudden onset of facial weakness or paralysis.
While the exact cause of Bell’s Palsy is unknown, several factors have been associated with its onset:
Viral Infections
Many cases of Bell’s Palsy have been linked to viral infections, such as:
Bell’s Palsy manifests suddenly, often reaching its peak intensity within 48 hours. The key symptoms include:
Facial Weakness or Paralysis
Clinical Evaluation
Diagnosis of Bell’s Palsy is primarily based on clinical presentation and the rapid onset of symptoms. Physicians typically conduct a thorough physical examination, focusing on the patient’s facial movements and reflexes. A detailed history is also taken to understand the onset, progression, and any preceding illnesses.
Excluding Other Conditions
Several conditions can mimic the symptoms of Bell’s Palsy, making differential diagnosis essential:
The treatment of Bell’s Palsy focuses on reducing inflammation, protecting the eye, and promoting recovery of the facial nerve. The management strategies include:
Corticosteroids
Corticosteroids, such as prednisone, are the mainstay of treatment for Bell’s Palsy. These medications reduce nerve inflammation and edema, improving the likelihood of a full recovery if started early—typically within 72 hours of symptom onset.
Antiviral Medications
Given the suspected viral etiology in many cases, antiviral agents like acyclovir or valacyclovir may be prescribed alongside corticosteroids. Although the benefits of antiviral therapy are still a matter of debate, some studies suggest that they may enhance recovery in patients with severe presentations.
Eye Care
Because Bell’s Palsy often impairs the ability to blink, protecting the eye on the affected side is critical:
Natural Course of Recovery
Most individuals with Bell’s Palsy begin to see improvement within a few weeks. Approximately 70% to 80% of patients recover completely or nearly completely within three to six months. However, recovery times can vary, and a small percentage of patients may experience residual weakness or other complications.
Factors Influencing Recovery
Several factors can affect the outcome:
Emotional and Social Impact
The sudden change in facial appearance can be distressing. Many patients report feelings of self-consciousness and anxiety, particularly in social settings. Psychological support, whether through counseling or support groups, can be beneficial in helping individuals cope with the emotional challenges posed by Bell’s Palsy.
Rehabilitation and Return to Daily Activities
Physical therapy not only aids in muscle recovery but also helps patients regain confidence in their facial movements. Occupational therapy may be recommended for those who experience difficulties with daily activities such as eating, speaking, or even smiling. Education about the condition also empowers patients to make informed decisions about their recovery and lifestyle modifications.
Long-Term Follow-Up
Regular follow-up with healthcare providers ensures that recovery is progressing as expected. In cases where recovery is incomplete or complications such as synkinesis develop, additional treatments such as botulinum toxin injections may be considered to improve facial symmetry and function.
Bell’s Palsy remains a condition that, despite its sudden and dramatic onset, has a generally favorable prognosis with proper treatment and supportive care. Understanding the anatomy of the facial nerve, recognizing the symptoms, and initiating early treatment are key components of effective management. While the exact cause of Bell’s Palsy is still under investigation, its association with viral infections and inflammatory processes offers a pathway for treatment that centers on reducing nerve swelling and protecting affected functions—especially vision.
Patients experiencing facial weakness should seek prompt medical attention to rule out other conditions such as stroke and to begin appropriate therapies. With a combination of corticosteroids, antiviral medications, and physical therapy, most individuals see significant improvement within a few months. Additionally, lifestyle modifications, stress management, and long-term follow-up are important aspects of recovery.
As research continues to advance, there is hope that more targeted treatments and preventive strategies will emerge. In the meantime, healthcare providers play a crucial role in not only managing the physical symptoms of Bell’s Palsy but also addressing the emotional and psychological impact that comes with the condition.
By understanding Bell’s Palsy in depth—from its causes and symptoms to its treatment and potential complications—patients and healthcare professionals can work together to ensure the best possible outcomes. Ongoing research and technological advancements in rehabilitation further enhance the prospects for recovery, offering optimism for those affected by this challenging condition.
This detailed report on Bell’s Palsy provides a thorough overview of what the condition entails, why it occurs, how it can be managed, and what patients might expect during recovery. Whether you are a patient seeking to understand your diagnosis or a healthcare professional looking for a comprehensive resource, the information outlined above aims to clarify the complexities of Bell’s Palsy while offering practical advice for managing and overcoming the challenges it presents.
BOOK APPOINTMENT